



|
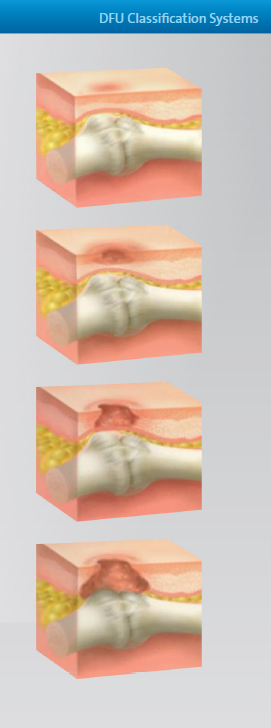
From DARCO India Innovation E-News, Issue 18, December 2017 Currently there are several classification systems known to specify a Diabetic Foot Ulcer (DFU). Some of them are very complex, some of them are too superficial, and some of them are simply not efficient.Jeffcoate stated in 2003(5) that "...there is no widely accepted method for classification or even describing foot ulcers. Non-specialists commonly refer to all ulcers as diabetic foot. Two international working parties are trying to define a system of describing individual ulcers to improve communication and develop a classification for audit and research. Without classification, selection of comparable populations for urgently needed multicenter trials will be impossible ..."(5). Such comments like "not widely accepted" or "not commonly used" appear all the way through the literature, even in the latest cited reference of 2012(24). In 2006 the Editors comment in Podiatry Today, Vol. 19 Issue 6 May(6), asked "Can a Diabetic Foot Surgery Classification System Help Predict Complications?" Researchers concluded that a non-vascular surgical classification system - including variables such as neuropathy, open wound and acute infection - may help predict peri- and postoperative complications. |
|
"...Armstrong believes the non-vascular diabetic foot surgery classifi cation system's framework may predict risk for complications such as amputation and infection ... just as it is best for one to be conversant in more than one language, it is best to be fluent in numerous classification systems ..."(6).
Generally speaking the Wagner and the UT seem to be the most commonly used (or at least known) classification systems, although or perhaps because they are already quite old.
Regardless which system is supposed to be the most accurate one, by the end of the day a classification system needs to have four advantages(9):
| › | Provides a valuable means for organization |
| › | Represents a common language for speaking with other medical professionals |
| › | Can help with reimbursement issues |
| › | Provides validation of chosen treatments |
© DARCO (Europe) GmbH
Download Literature: "DFU Classification Systems Literature Review" (PDF)

|
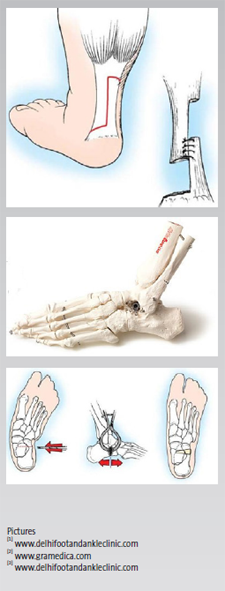
From DARCO India Innovation E-News, Issue 17, September 2017 Gait Training - essential to use an off-loading shoe correctlyHindfoot relief can remove the entire load from the heel while providing targeted relief to specific areas through cushioning and/or additional customizable insoles. Great caution must be taken when treating patients with neuropathies!*As long as the upper and lower ankle joints are properly aligned, plantar ulcers of the heel / calcaneus are often forced by foreign bodies (i.e. little stones in the shoe) and shear force, especially in Hawaiin style sandals. Also, deformities with intrinsic bone spurs might create high peak pressure point. Usually in human gait after the swing phase, the first ground contact is done with the heel. In case of injuries, ulcers, pain, etc. this first heel strike needs to be avoided. An off-loading shoe can do this, but the patient also needs to get advised and perhaps trained to change his normal gait during the healing process. Patient must be taught to walk correctly in this device as gait pattern must be altered to reduce trauma to heels. Like in some running styles patients need to have first initial contact with the forefoot. This changed gait will also shift some load further to the forefoot. Therefore additional injuries or ulcers on the forefoot are a contraindication for such an off-loader. Also be careful in the use of these rear foot off-loaders in the case of achilles tendon injuries. So "forefoot-gait" might also put some additional tension on this area. Additional helping aids might be required such as height adjustment shoes on the contralateral side or crutches. As a conclusion: especially with off-loading shoes the patient education / gait training must be regarded as an important aspect of the whole healing process. © DARCO (Europe) GmbH |

|
Literature:
*Baumgartner et al (2016) "Pedorthics" | C. Maurer publisher, Geislingen, Germany

|
From DARCO India Innovation E-News, Issue 16, June 2017 Although Orthotics and stretching are effective, some young patients may require a surgical correction ...A pediatric flatfoot can be caused by a variety of reasons and surgical therapy may be indicated. The catch is to correct the hindfoot without impacting the structures and alignment of the forefoot.Soft Tissue Procedure
Subtalar Implants
Evans procedure |
|
Postoperatively and in most cases, a cast might be required. This is especially true for younger patients (kids). Recovery time can be anything between six to eight weeks. An adequate cast shoe or post-op shoe with a rocker sole will help to mimic the normal gait during the healing process.
© DARCO (Europe) GmbH
Literature:
Baravarian, Babak, Assistant Professor at UCLA, Santa Monica
in Podiatry Today, Volume 23 - Issue 1 - January 2010

|
From DARCO India Innovation E-News, Issue 15, March 2017 How useful can a hybrid between a Wound Care Shoe and a Diabetic Shoe be?In newsletter No. 6 we discussed the advantages of the toe/heel rocker bottom coupled with a flat midstance area for the neuropathic patient. In newsletter No. 8 we pointed out the advantages of a light weight diabetic shoe; the GentleStep™. By combining the features of both models we've created a very effective hybrid.Patients at risk of developing diabetic foot ulcers need to avoid getting foreign objects in their shoes, such as sand or little stones. Such objects may irritate or even harm the skin and this increases the chance of getting a foot ulcer. A closed-toe shoe is therefore recommended. The shoe should have a wide toe box and made with a breathable fabric. The upper material needs to be strong enough to protect, yet flexible in order to reduce dorsal pressure; especially in the case of hammer toes. Once an ulcer exists, it is crucial that the footwear allows for selective off-loading. Customizable, multilayered, insoles with different foam densities can be carefully altered to off-load the wounded area and redistribute the weight. WAGNER grade 3 or 4 ulcers are severe and therefore also require a shoe with a wide opening to accommodate the thick dressings. For example our sandal style of shoes; the WCS™. Regardless whether an ulcer has manifested, individuals at risk would still benefit from a multilayered, customizable insole system. Combining the advantages of the WCS™'s outer and insoles systems, together with the friendly upper material found in the GentleStep creates a superior, versatile therapeutic shoe treating WAGNER 1 or 2 ulcerations. WCS™ Closed Toe shoe has a closure system that cannot expose the entire interior of the shoe, as found with the WCS™ Open-Toe model. Therefore in the case of very bulky dressings, the WCS™ Open-Toe model should be the first choice. Keep in mind that the off-loading capabilities of both models are identical. In addition, there's a small marking located on the medial aspect of the outer sole; the DARCO "D". This insignia indicates the correct position of the first metatarsal and facilitates proper fitting of the shoe. An ill-fitting shoe may actually do more harm than good. © DARCO (Europe) GmbH |
|

|
From DARCO India Innovation E-News, Issue 14, December 2016 Testing for Diabetic
|
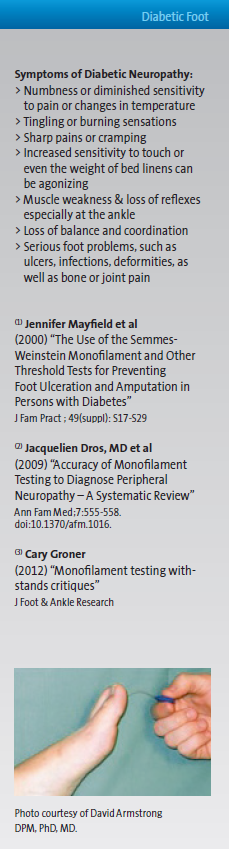
|

|
From DARCO India Innovation E-News, Issue 13, September 2016 Conservative Treatment
of a Bunion (Hallux Valgus) -
|

|
Literature:
Wanivenhaus, A., Vienna, (2015) "Hallux Valgus konservativ behandeln - geht das?"
JATROS, Ortho-Rheuma-Spezial, No2/S.78

|
From DARCO India Innovation E-News, Issue 12, June 2016 Is there a biomechanical need for the use of a counter side height adjustment while wearing a Wedge Shoe?By wearing a wedged post-surgical or off-loading shoe, the patient will experience a bilateral asymmetry in leg length which leads to a limping gait. Patients might claim knee, hip and/or lower back pain after wearing a wedged shoe for a while due to a changed biomechanical function chain.It looks like the human body can tolerate a leg length difference up to 2 cm (1). Differences of more than 2 cm can lead to difficulties in walking. Even patients without diabetic ulcers and/or neuropathy often claim pain in the Sacroiliac Joint. In Berlin Germany, Dr. Edelmann observed 100 patients in a period of 8 months who underwent a Hallux Valgus correction surgery and had to wear a forefoot off-loading shoe.
In 1991 McCaw et al (2) described the biomechanical implications of mild leg length inequality and pointed to
In 2013 O'Leary et al (3) did a systemic literature review and came to the conclusion that foot & ankle deviations can be considered a potential cause of lower back pain. A height adjustment, i.e. in the form of a height difference shoe, can therefore be considered an important part of the complex treatment of foot & ankle disorders. © DARCO (Europe) GmbH |
|
Literature:
Burke Gurney, PhD, PT, et al, Effects of Limb-Length Discrepancy on Gait Economy
and Lower-Extremity Muscle Activity in Older Adults
J Bone Joint Surg Am, 2001 Jun; 83 (6): 907 -915 . http://dx.doi.org/
(2) McCaw et al, Biomechanical implications of mild leg length inequality
Br J Sp Med 1991; 25(1) 10-13 http://bjsm.bmj.com
(3) O'Leary et al, The effects of podiatrical deviations on nonspecific chronic low back pain
J Back and Musculaoskeletal Rehabilitation, 2013, (26) 117-123 IOS PressDOI 10.3233/BMR-130367

|
From DARCO India Innovation E-News, Issue 11, March 2016 When a TCC treatment is needed, protection of the cast and gait support is importantAn earlier Newsletter (No. 7/2015) offered a literature overview on CAM Walkers as an alternative to the TCC. Physicians seek to achieve the best results based upon indications and within the confines of available resources. Therefore, a natural or synthetic cast may be the best solution at hand.Orthopedic casts were first developed in the 1850s and their aesthetics haven't changed much over the past 160 years. A cast can be used to brace, immobilize, protect as well as off-load at and around the foot and ankle, hence providing effective treatment for many indications. Fiberglass replaced plaster in the 1970s and waterproofing arrived in the '90s. Walking on a cast without protection can lead to cast damage and other complications. Foreign bodies can find their way through the sole of the cast (pic1 & 2), and the toes are exposed and unprotected. In the 1950s, rubber heels were invented and are still often used today (pic3). The rubber walking heel prevents direct contact of the cast with the ground and is designed to make the gait more comfortable. But the height difference can lead to biomechanical stress and may interfere with a normal gait cycle. This can be avoided with a height compensation shoe (pic4). The abnormal walking pattern often leads to lateral rotation affecting the ankle joint. This is especially true after several days as the cast loosens around the calf due to muscle atrophy. Self-Repair strategies are often seen, including "shoe-like" improvements (pic4 & 6). These improvements can easily be achieved with an off-the-shelf cast shoe, which not only provides protection, but can also allow the patient to experience a normal gait cycle as much as possible while wearing a cast. |

|
© DARCO (Europe) GmbH
References:
Pic 1: By courtesy of Dr. Rajesh Kesavan, Chennai, India
Pic 2: Edmonds, M, A practical Manual of Diabetic Foot Care, Blackwell, 2008
Pic 3: Rubber Heel https://lh3.googleusercontent.com/-OhBtY6qK2ls/VXc28psTpWI/AAAAAAAAAJI/
UnrY3AEfZ9E/w506-h380/SLWC2.jpg
Pic 5 & 6: http://travelogue.travelvice.com/romania/crippled-couchsurfer-romanian-x-ray-experience/

|
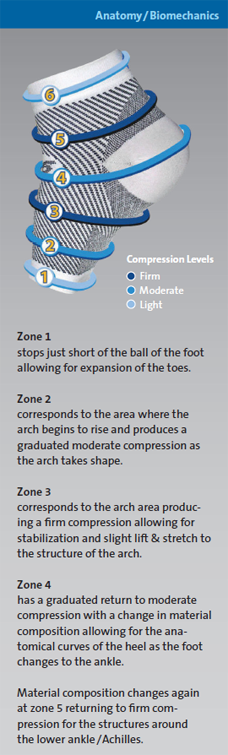
From DARCO India Innovation E-News, Issue 10, December 2015 The importance of treating edema in Plantar Fasciitis conditionsIn newsletter No. 5 we explained briefly the condition of a plantar fasciitis. Night splints are a treatment option with high healing potential. But what about wearing an additional device to support healing during the day?According to A. Jacobs(1), 21 % of patients with plantar fasciitis are also subject to swelling and edema. And of these patients he identified a small group as having plantar fascial fibromatosis (Morbus Ledderhose). Although a true Morbus Ledderhose is less common, it usually occurs in the middle and medial part of the plantar aponeurosis(2). In the Jacobs findings, 25 % of all plantar fasciitis cases experience some kind of fibromatosis. The final 54 % of those suffering from plantar fasciitis were related to degenerative conditions cause by age and/or overuse. In this group, there was an occurrence of microscopic and tiny tears in the plantar aponeurosis, which can eventually lead to partial rupturing. A compression sleeve can address the edema issue and due to the different compression areas in the sleeve, an increased support of the medial arch can also be achieved. One can also support of the medial arch with orthotics and/or by adding a soft padding to the heel area. For an effective compression sleeve, different compression zones are needed to facilitate the proper flow of fluids without constricting circulation. In order to support the medial arch, a higher compression is needed around the base of the metatarsal bones. Using the same manufacturing process for medical compression stockings, six different zones with varying levels of compression were designed into this Foot Sleeve to strengthen and support the natural foot structures. The end zones on most tight compression garments prove to be troublesome due to the sudden and abrupt increase of pressure, causing an "edge" effect that can lead to an increase in edema where the garment itself stops, which is not the case with the DCS. |
|
© DARCO (Europe) GmbH
Literature:
A. Jacobs, (2013) "An Evicence Based Medicine Approach to Plantar Fasciitis",
Podiatry Today. Vol 26 (11)
Sharma S, (2003) "MRI diagnosis of plantar fibromatosis - a rare anatomic location",
The Foot 13 (4): 219-22. doi:10.1016/S0958-2592(03)00045-2

|
From DARCO India Innovation E-News, Issue 9, September 2015 R.I.C.E. vs. M.E.A.T.
|
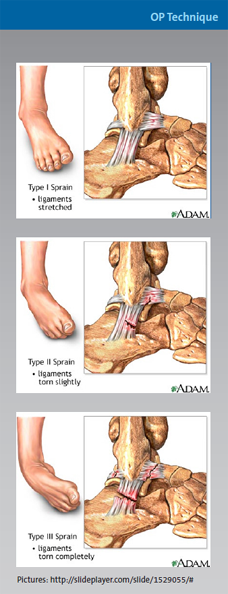
|
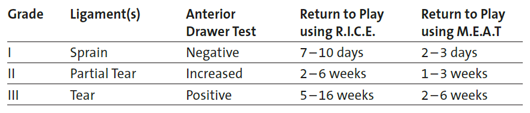
So if you suffer from a grade II or III ankle sprain, don't neglect to consult your physician.
© DARCO (Europe) GmbH
Literature:
Tseng CY1, Lee JP et al, (2013) "Topical cooling (icing) delays recovery from eccentric exercise-induced muscle damage"
J Strength Cond Res. May;27(5):1354-61. doi: 10.1519/JSC.0b013e318267a22c
* Rest - Ice - Compression - Elevation
** Movement - Exercise - Analgesics - Treatment

|
From DARCO India Innovation E-News, Issue 8, June 2015 One fits all?
|

|

|
From DARCO India Innovation E-News, Issue 7, March 2015 Total Contact Cast (TCC)
|
|

Please visit our India E-News archive to see more publications on Expertise